A thymectomy is the process of removing the thymus gland, which lies under your breastbone (also called the sternum). This gland helps your immune system develop during childhood but usually shrinks with age.
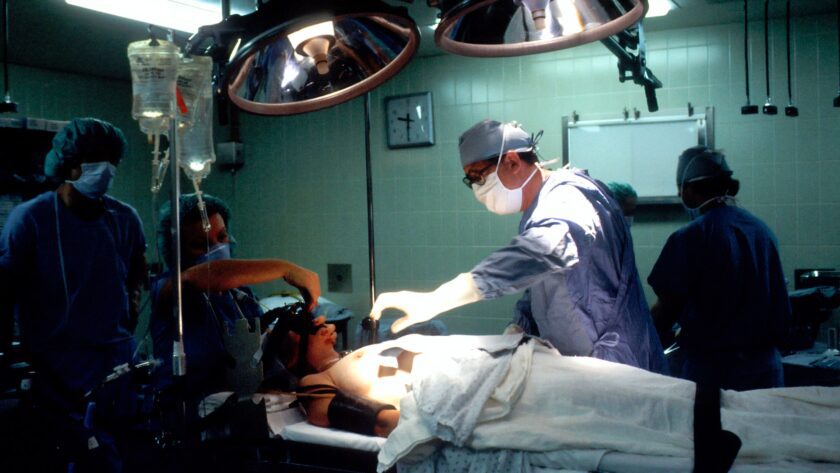
The procedure is done under general anesthesia. We usually perform a transcervical thymectomy, which involves an incision in the neck.
What is a Thymectomy?
A thymectomy is surgery to remove the thymus gland. This is under the breast bone and helps your immune system develop during childhood. If you have MG, the thymus can become inflamed and cause muscle weakness. Thymectomy reduces or eliminates symptoms in 60% of patients with myasthenia gravis and often results in permanent remission.
During the surgery, you will be put under general anesthesia that will make you asleep throughout the operation. Let me know if you need any further assistance. The surgeon, like Armen Parajian, will choose one of several surgical approaches:
A transcervical or a transsternal approach is the most commonly used technique. These involve a cut on the chest wall (sternum) and removal of the thymus and adjoining fat. This surgery is considered more invasive than other surgical options for myasthenia gravis and may be associated with more extended hospital stays, increased morbidity, and complications.
What is the Procedure?
A thymectomy is usually performed as an open surgery. This means that the surgeon will make an incision through the skin over your breastbone (sternum) and then divide it to expose the thymus and remove it. This is the most common way to do a thymectomy.
There are also less invasive techniques for removing the thymus. These include video-assisted thoracic surgery (VATS) and robotic-assisted thoracoscopic thymectomy. Both use a tiny camera that sends images to a monitor and special surgical tools inserted through other incisions.
Your MG specialist and surgeon will review your options and recommend the best type of surgery for you. Depending on your situation, this could mean a trans-sternal thymectomy, a VATS minimally invasive approach, or a robotic thoracoscopic approach.
How Long Will I Need to Stay in the Hospital?
If you have MG, your doctor may recommend thymectomy, especially if your acetylcholine receptor antibodies are high. In most patients, thymectomy significantly improves muscle weakness and reduces medication need. In some cases, thymectomy can even lead to permanent remission.
There are several surgical approaches for thymectomy. The most common involves cutting through the anterior chest (sternum) and removing the thymus and any adjoining fat. Other surgeons prefer a less invasive approach, including using video-assisted thoracoscopy or robot-assisted thoracic procedures.
These techniques involve smaller incisions and a camera with flexible arms to view the operation. Chest tubes drain any fluid build-up in the chest and help the wound heal. Following the surgical procedure, the patients must stay in the hospital for a few days.
How Will I Feel After Surgery?
Pain will vary after surgery depending on the type of thymectomy and your medical history. During recovery, your doctor will prescribe or recommend a course of pain medication to help control the discomfort you experience.
After the thymectomy, your doctor will ask you to breathe deeply and cough repeatedly to clear your lungs of mucus. Medications to open the lungs and make breathing easier may also be used.
You might have some muscle pain in your chest, neck, or back from lying on the operating table. You might also have some throat pain. It’s a good idea to let friends know you’ll miss school for a few days so they can take notes and drop off assignments. It is essential to take antibiotics as prescribed to avoid infection and prevent complications after surgery.
What Can I Expect from My Surgeon?
When you’re choosing a surgeon to perform your thymectomy, look for one with expertise in myasthenia gravis. They’ll review your medical history and examine you before making a recommendation.
They may recommend a trans-sternal or keyhole (video-assisted thoracoscopic) approach to remove the thymus. With a trans-sternal surgery, the surgeon will open the breastbone (sternum) and remove the thymus and adjoining fat.
With video-assisted thoracic surgery, the surgeon will make several tiny incisions. They’ll insert tools, including a robotic arm, through the incisions to remove the thymus. They’ll close the incisions with stitches. This minimally invasive technique results in shorter hospital stays and faster patient recovery. It also reduces postoperative pain and complications. You can return to work after six weeks with either type of procedure.